| Category | SLAP Repair |
Arthroscopic SLAP repair (Superior Labral Repair)
This is a keyhole operation performed under general anesthesia and regional nerve block. Tiny (<1cm) incisions allow the introduction of the arthroscope, instruments, and implants.
A tear in the superior labrum is often called a SLAP tear. This term stands for 'Superior Labrum Anterior and Posterior (to Biceps tendon)'. Injuries to the superior labrum can be caused by acute trauma or by repetitive shoulder motion. An acute SLAP injury may result from:
People who participate in repetitive overhead sports, such as throwing athletes or weightlifters, can experience labrum tears as a result of repeated shoulder motion.
Many SLAP tears, however, are the result of a wearing down of the labrum that occurs slowly over time. In patients over 30 to 40 years of age, tearing or fraying of the superior labrum can be seen as a normal process of aging. This differs from an acute injury in a younger person.
Symptoms
The common symptoms of a SLAP tear are similar to many other shoulder problems. They include
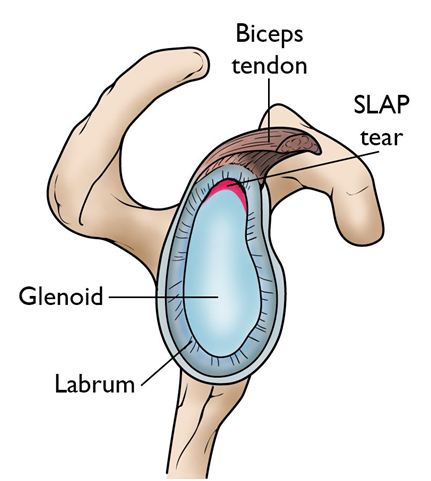
This cross-section view of the shoulder socket shows a typical SLAP tear.
The superior labrum and the origin of the long head of your biceps tendon are intimately related, so the symptoms of both can overlap, and sometimes a tear of the superior labrum is best treated by disconnecting the long head of the biceps tendon from the glenoid socket.
Your pattern of superior labral injury is assessed to decide which treatment option is best for you:
SLAP Repair
The torn superior labrum is mobilized from scar tissue. The exposed upper glenoid bone is prepared to optimize healing using a rasp or a burr and your superior labrum is reattached to the bone using suture anchors (as shown below).
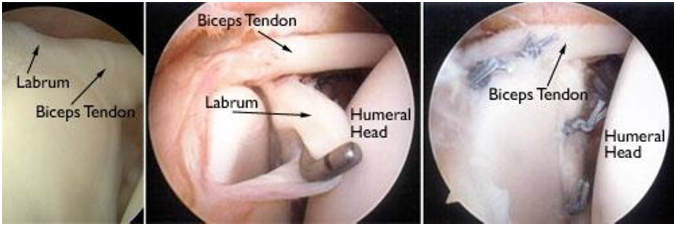
(Left) An arthroscopic view of a healthy labrum. (Center) In this image, the surgeon uses a small instrument to evaluate a large SLAP tear. (Right) The labrum has been reattached with sutures.
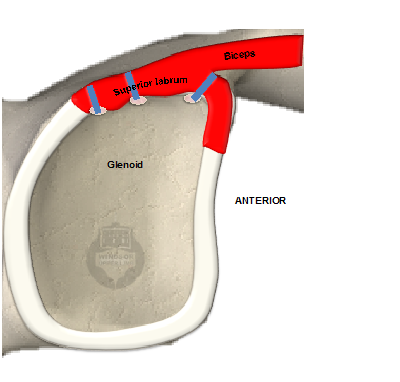
Superior labrum is repaired to the glenoid using suture anchors
What is my recovery after surgery?
You will usually go home on the same day as your operation. Please take your painkillers regularly for the first few days and begin them before your nerve block wears off.
You will need to wear a sling for six weeks. Your physiotherapist will guide you through your rehabilitation. After 6 weeks you will progress to active shoulder motion and you will begin to strengthen from 10 weeks. All restrictions will be removed within 6 months.
You can take down bulky padded dressings on day 2 after surgery, but keep your wound dry and covered with your waterproof dressings for 12 days. You can shower for 4 days with waterproof dressings on.
Patients vary in their symptoms after surgery, but in general, you can expect to return to:
By six months, 85% of patients will feel their shoulder is better. You may notice some stiffness in your shoulder, but this usually improves over the first year of your operation.
When will I be followed up?
You will be seen two weeks after your operation. Depending on your progress, your ongoing follow-up will vary, but many patients can be discharged between six months and twelve months after surgery.